In recent decades in the United States, discussions around mental health struggles have become less stigmatized. A study in the journal, Health Affairs, found that this is likely due to a combination of increased media exposure, increased employer recognition of these issues, and the continued efforts of public education programs conducted through mental health organizations. However, the same study noted that while mental health as a subject has benefitted from more awareness, many Americans face a lack of resources for treatment – particularly due to the immense deinstitutionalization that has occurred over the last several decades.
At United Way of the National Capital Area, we are aware of how the issue of mental health intersects with other social issues, including race, poverty, homelessness, domestic abuse, and more. For example, according to one study of adults with a diagnosis-based need for mental healthcare, 37.6% of White people received treatment, compared to only 22.4% of Latinos and 25.0% of Black people.
Part of our health initiative is to bring these inequities to light and continue to discuss them. One area we wanted to focus on was the accessibility of treatment in the mental health sphere. With so much of mental health and treatment changing due to COVID-19, and in honor of Minority Mental Health Awareness Month in July, we wanted to conduct a data study of mental healthcare access and attitudes across the United States. Below are our full findings.
Major Insights
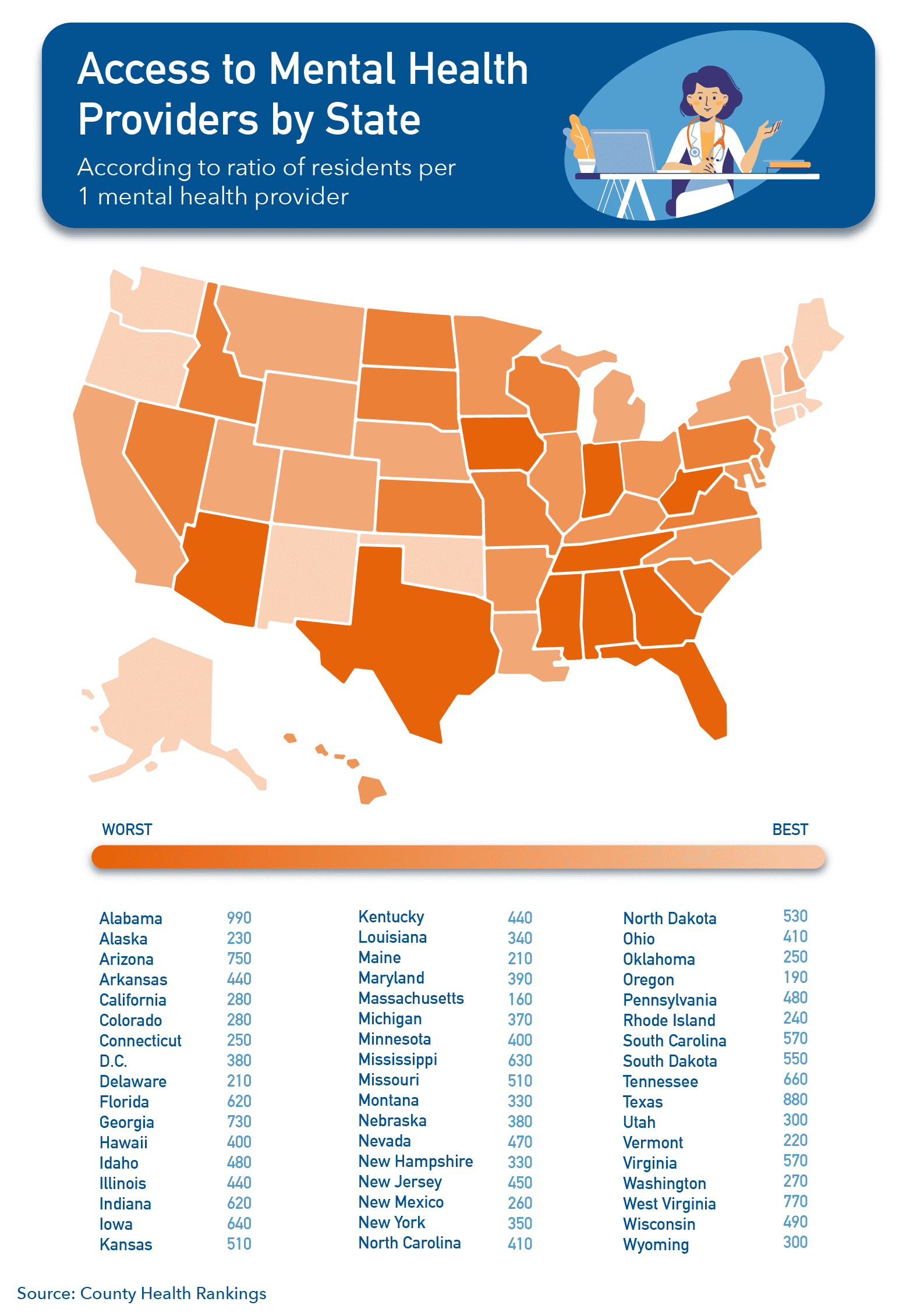
- – The Southeastern portion of the United States has the highest resident to provider ratio, making mental health resources in these areas the least accessible in the country.
- – 22% of Americans feel uncomfortable accessing mental health resources should they or a loved one need them.
- – Telehealth appointments may make mental health resources more accessible, but they do not necessarily change how comfortable patients feel accessing them. 27.71% of Americans feel more uncomfortable accessing virtual resources than in-person ones.
Study Methodology
In order to illuminate the gaps in receiving quality mental healthcare in the U.S., our study includes:
- – An analysis of access to mental health providers by state, according to County Health Rankings
- – Attitudes around accessing mental healthcare (by state, gender, and age), according to a survey of 2,500 Americans in June 2020
- – Attitudes around accessing virtual mental healthcare versus in-person treatment (by state, gender, and age), according to a survey of 2,500 Americans in June 2020
Gaps in Mental Healthcare Access by State
According to data compiled by County Health Rankings, some parts of the United States have a very high ratio of residents to mental healthcare providers. This is particularly a problem in the South, where the worst ratios seem to be most concentrated. For example, Alabama has 990 residents to one mental healthcare provider. Texas has a ratio of 880:1, and West Virginia comes in third with 770:1.
The States with the Best Mental Health Services (Most Access)
-
- Massachusetts
- Oregon
- Delaware
- Maine
- Vermont
- Alaska
- Rhode Island
- Connecticut
- Oklahoma
- New Mexico
The States with the Worst Access to Mental Healthcare Providers
-
- Alabama
- Texas
- West Virginia
- Arizona
- Georgia
- Tennessee
- Iowa
- Mississippi
- Indiana
- Florida
Not having access to care is a significant barrier to receiving proper mental health treatment. As cited by County Health Rankings, “access to care requires not only financial coverage, but also access to providers. Thirty percent of the U.S. population lives in a county designated as a Mental Health Professional Shortage Area.”
Attitudes Toward Mental Healthcare in the U.S.
Another significant barrier to mental healthcare is stigma, whether social or internal. We know that many minority groups are less likely to seek out mental healthcare due to community stigma. We wanted to conduct a survey to see how those opinions vary on a state level in the United States. So we asked 2,500 Americans: how comfortable do you feel accessing mental health resources (in-person, virtual, hotlines, etc.) if you or a loved one should need it?
According to our findings, a total of 34.06% of Americans feel comfortable (combined somewhat comfortable and very comfortable) accessing mental health resources. 22.01% feel uncomfortable (combined somewhat uncomfortable and very uncomfortable) and 22.93% feel neither comfortable nor uncomfortable. We compiled a list of the states that feel the most uncomfortable seeking mental healthcare below.
The States Where Residents are Least Likely to Seek Mental Health Care
- Vermont
- Mississippi
- Colorado
- New Jersey
- West Virginia
- Kansas
- Ohio
- D.C.
- Idaho
- Wyoming
To view the results of the survey in detail for each state, hover over each segment in the below interactive chart.
Now, why does this matter? For context, we decided to determine if there was a correlation between these two variables. Does an increase in access to mental healthcare providers correlate to an increased comfort level in accessing them? In the below graph, you can see that our data suggests it does.
While we cannot say that more access causes increased comfort levels around receiving care, you can see in the graph that the higher the ratio of residents to providers, the higher the discomfort levels in that area. Kind Seeds explains that this could be due to a number of factors, i.e. more access may mean less stigma in that area, and more access typically indicates an increase in other factors in that geography, such as less poverty, more insurance coverage. It’s clear to us that we cannot effectively encourage individuals to seek the treatment they need without providing their local healthcare communities with the proper resources to help.
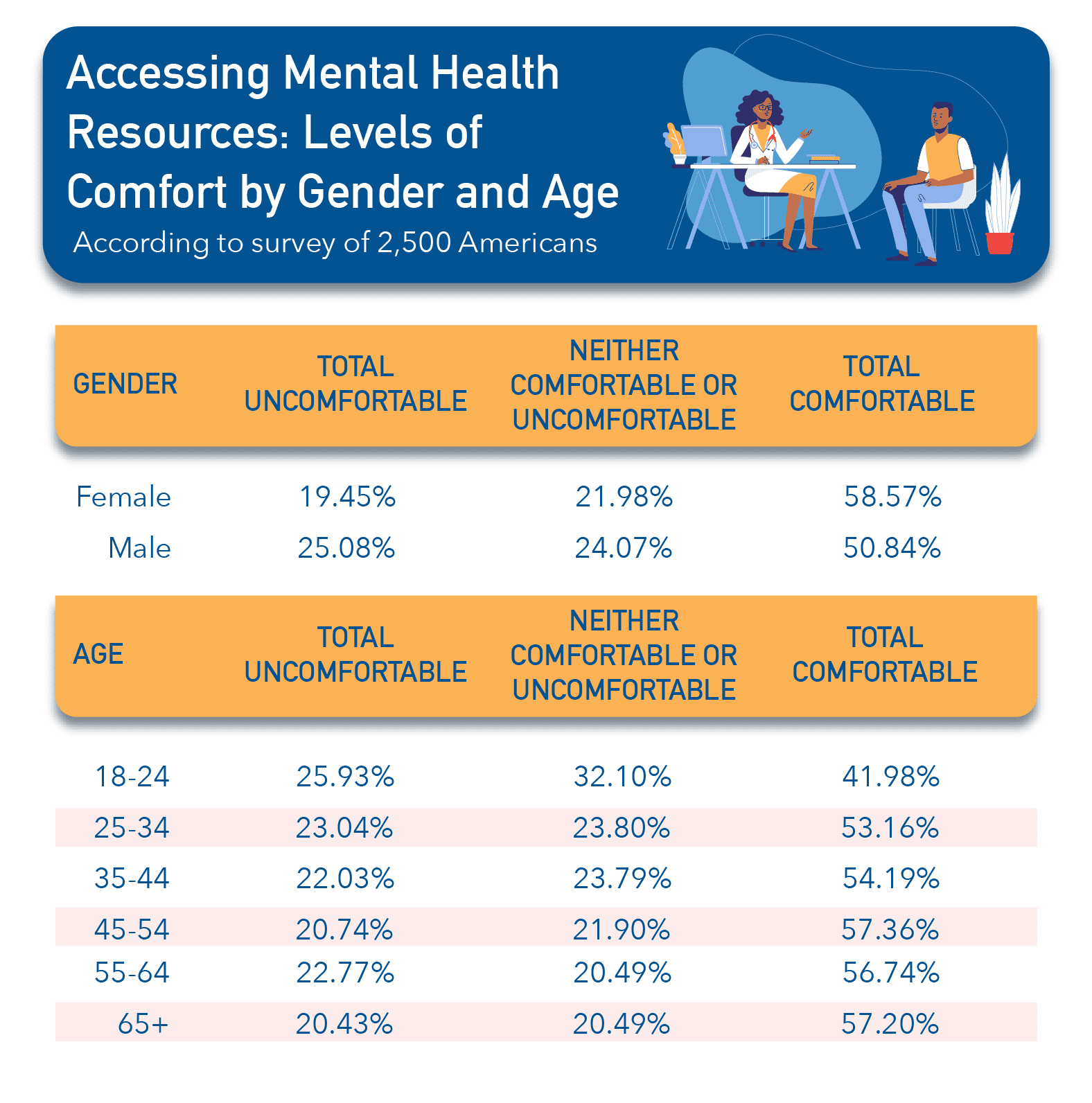
We also wondered how these results differed by age and gender. According to our findings, women reported feeling comfortable accessing mental healthcare 7.73% more than men. And surprisingly, despite the continued destigmatization of mental health topics over time, young people aged 18-24 were the group most uncomfortable with accessing mental health resources (25.93%). Our full results are illustrated in the table below.
Attitudes Toward Virtual Mental Healthcare in the U.S.
Over the past several months, and out of necessity, healthcare models have moved toward making telehealth a priority. Many predict the change will be long-lasting and change how we view care and treatment for years to come. We wondered: how would the potential to access a virtual mental healthcare model affect the numbers we were seeing above? Telehealth certainly addresses issues of access, but do those who need treatment feel comfortable using it?
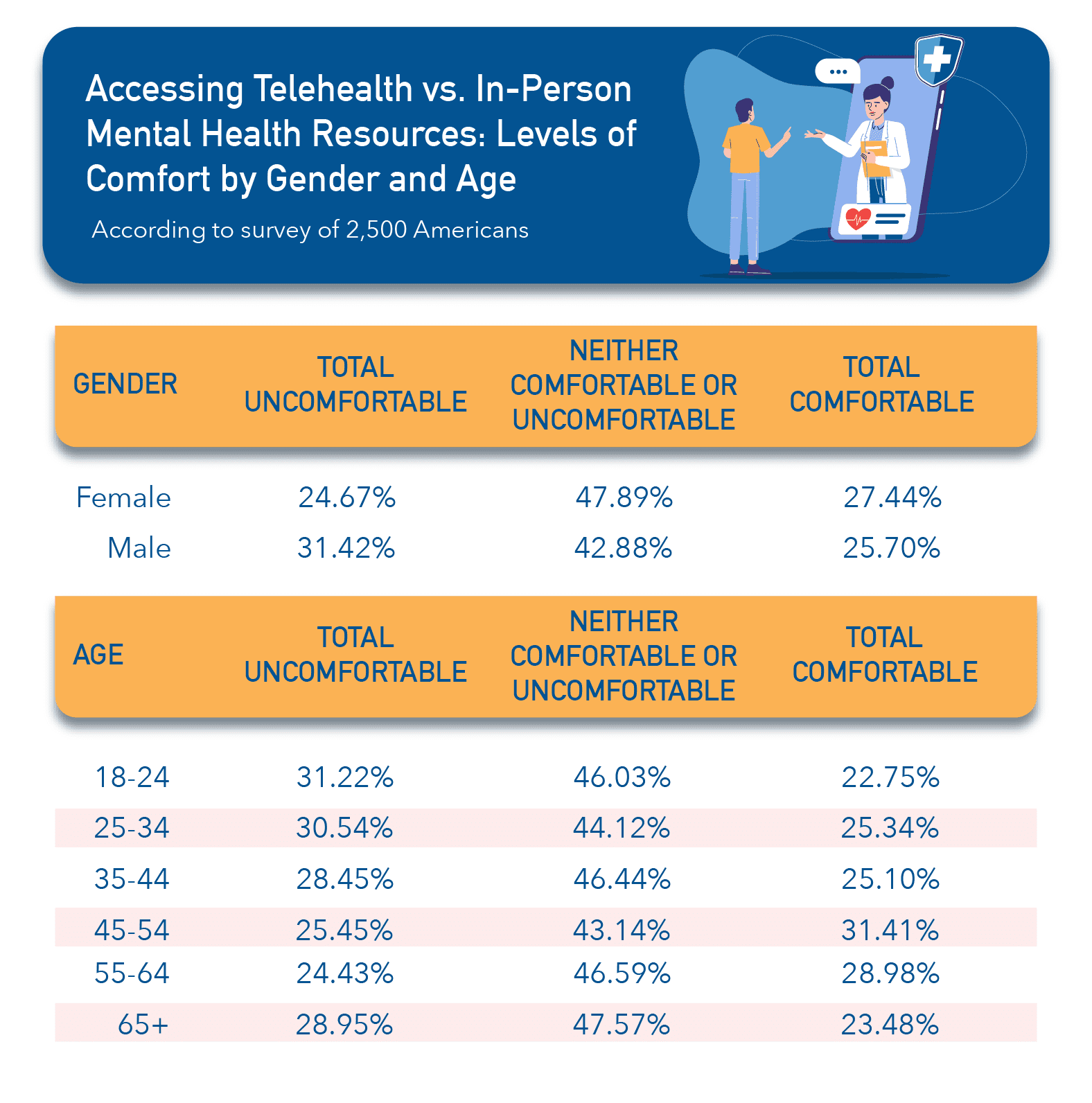
We conducted another survey, asking 2,500 Americans: relative to in-person resources, how comfortable do you feel accessing virtual mental health resources, such as telehealth therapy sessions?
According to the results, Americans seem to be split on this topic. Only 26.65% of our respondents feel more comfortable accessing virtual resources than in-person ones for mental healthcare (combined somewhat more comfortable and much more comfortable). On the flip side, 27.71% feel more uncomfortable accessing virtual resources (combined somewhat more uncomfortable and much more uncomfortable).
In fact, it seems that most Americans don’t view virtual mental healthcare as the saving grace of mental healthcare access, as 45.63% feel it doesn’t impact their comfort level accessing mental healthcare at all. However, this data varied state by state. Below are the states that feel least comfortable with virtual mental health care.
The States Where Residents are Least Likely to Seek Virtual Mental Health Care
- Mississippi
- Maine
- North Carolina
- Virginia
- Tennessee
- Rhode Island
- Michigan
- New Mexico
- Wyoming
- Massachusetts
Similar to our first survey, we wondered how these results differed by age and gender. In summary, we saw a similar pattern in gender, where men are much more likely to be uncomfortable accessing virtual mental health resources. Interestingly, there seems to be no real pattern among different age groups when it comes to virtual mental health. It’s likely up to the individual’s comfort level with technology, as groups aged 18-34 were some of the least comfortable with telehealth, along with (predictably) the group aged 65+.
 Going Forward
Going Forward
What does all of this mean for mental healthcare access in the United States? Regardless of new developments in technology, increased access to quality mental healthcare remains a priority. The COVID-19 pandemic has only exacerbated existing stressors such as unemployment, poverty, and eviction –stressors that are disproportionately faced (even in non-pandemic times) by communities of color. Pandemic-related stress along with the loss of healthcare coverage for an estimated 27 million Americans due to the recent economic downturn and uptick in unemployment are also issues that disproportionately affect marginalized populations, who often also experience medical discrimination and other traumas. In short, the need for trauma-informed, accessible mental health care is increasingly evident.
At United Way of the National Capital Area, we are focused on equity across all areas, including mental healthcare. Learn more about what you can do to support our health and wellness initiatives here.